Surgical Sperm Retrieval
- Consultations
- Initial Consultation
- Fertility Assessment
- Fertility Treatments
- In-Vitro Fertislisation (IVF) & Intra – Cytoplasmic Sperm Injection (ICSI)
- Frozen Embryo Transfer (FET)
- Intra Uterine Insemination (IUI)
- Surgical Sperm Retrieval
- Egg Freezing
- Sperm Freezing
- Endometrial Scratch
- Embryo Glue
- EmbryoGen

This patient information aims to provide you with information regarding surgical sperm retrieval (SSR). The information below is general. The precise reasons why you have been suggested SSR will be discussed with you in clinic and you should feel free to ask any questions about your procedure and or reasons for having it.
What is SSR?
Sperm are produced in the testicles, and stored in the epidydimis before being ejaculated when the man has an orgasm. For some men, despite having sperm production, no sperm are ejaculated and hence he suffers from azoospermia. Using SSR techniques it is possible to extract sperm directly from the site of production (testicles) or from the site of storage (epidydimis).
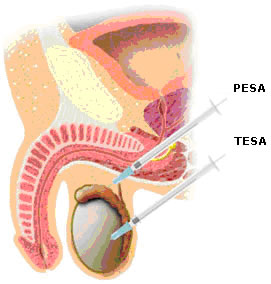
PESA (percutaneous epidydimal sperm aspiration) is when a small needle is used to collect sperm from the epidydimis.
TESA (testicular sperm aspiration) is extracting sperm from the testicle using a small needle.
TESE (testicular sperm extraction) is taking a small biopsy from the testicle.
The SSR, depending on type, is generally performed under conscious sedation or local anaesthetic. If sperm are present they are either frozen for subsequent use or prepared and used directly in fertility treatment called ICSI-IVF. A single sperm is injected into oocytes to achieve fertilisation. Normal fertilisation occurs in about 60% of the eggs, and embryo(s) are later transferred back to the treated woman with the aim to achieve a pregnancy as in a standard IVF treatment cycle.
Before SSR
We always offer freezing of any sperm found after SSR. Before sperm can be frozen, we need to have written consent from you. We also need to screen you for infectious diseases (HIV, Hepatitis B and Hepatitis C). All screening needs to be negative for us to be able to store your sperm. Therefore, the embryologist will arrange consent taking and screening prior to SSR to inform you about sperm storage, treatment options, and terms and conditions.
You should consider the following questions:
- How long do I want to have my sperm stored for?
- What do I want my samples to be used for? For example, use in fertility treatment with your wife or partner, or use for research.
- What do I want to happen to my samples if I die?
- You can change the terms of the storage at any time, but you must do this in writing. You may want to do this if your circumstances change (for example a change of partner) or if you just change your mind.
On the day of SSR
You should not have anything to eat for 6 hours prior to the procedure. On arrival to our unit, you will be shown to a room and asked to change into a gown. Your partner (if applicable) may accompany you to the room, but not join you in theatre for the procedure. In theatre you will be sedated by the anaesthetist. The doctor will perform the surgical sperm retrieval and the embryologist will examine the tissue or fluid for the presence of sperm under a microscope.
At the end of your procedure, as you are starting to wake up, you will be given a Voltarol suppository for pain relief. This will be inserted into your rectum. The effects will last for 12 hours; therefore you should avoid painkillers containing ibuprofen during this time.
Following this you will return to the room and rest for a short while, before being discharged. You will be a little drowsy from the sedative drugs and you must be accompanied home. You must not drive for 24 hours.
After SSR
You may experience some discomfort following the procedure which should be relieved by simple painkillers. We advise that you wear supportive underwear and loose trousers until the discomfort has settled.
You will receive a letter from us explaining the findings from the SSR and expiry dates if we were able to find and store sperm.
Issues to consider
Not all patients are suitable for SSR
Prior to considering SSR we will examine you thoroughly with a physical examination, chromosome analysis and hormone level screening. The findings will indicate how likely a SSR is to be successful for you. Sometimes the findings of the investigations will mean that you are not a suitable candidate for this procedure.
We understand that this might be very disappointing, but undergoing a surgical procedure will very low chances of success is not in your best interest.
Not all patients having a SSR will have sperm production
Sometimes the investigations prior to the SSR have been positive, indicating a good chance of finding sperm. Despite this, we sometimes fail to find sperm. There could be many reasons for this; one is localised sperm production which means that there could be local areas within the testicles that are producing sperm but that the biopsy sample failed to retrieve the sperm. Alternatively, the SSR may be done for closure, with less hope of finding sperm. We understand that in both circumstances this will be disappointing.
Not all sperm are suitable for freezing
In general, around 50% of sperm survive the freezing and thawing process. Low quality sperm tend to tolerate the procedure less well. We cannot guarantee that any sperm found will survive the process.
Not all sperm are capable of fertilisation
The sperm retrieved from the testicle or from the epidydimis may not be fully mature. The average fertilisation rate using testicular sperm is around 60%. If sperm are not fully mature, the chances of fertilisation will be lower. We cannot guarantee fertilisation, pregnancy or live birth using SSR sperm.
Are there any risks with an SSR?
The biopsy procedure carries a small risk of bruising and infection to the biopsy site. In addition, there is a small risk of haematoma, acne, tethering of skin and testicular failure. These risks will be discussed with you by the clinician.
Further information
If you have any questions or would like further information, please contact us.
TESTIMONIALS
Mr Brook, Reception Staff and Nurses, friendly, efficient, and caring. Supportive and understanding.


