In-Vitro Fertislisation (IVF)
- Consultations
- Initial Consultation
- Fertility Assessment
- Fertility Treatments
- In-Vitro Fertislisation (IVF) & Intra – Cytoplasmic Sperm Injection (ICSI)
- Frozen Embryo Transfer (FET)
- Intra Uterine Insemination (IUI)
- Surgical Sperm Retrieval
- Egg Freezing
- Sperm Freezing
- Endometrial Scratch
- Embryo Glue
- EmbryoGen

What is in vitro Fertilisation?
'In vitro fertilisation' means fertilisation outside the body. It is a method that has helped many women to have babies since 1978 when it was first used successfully. IVF treatment is now offered in many UK clinics, all of which are licensed and monitored by the Human Fertilisation and Embryology Authority (HFEA).
IVF involves the collection of oocytes (eggs) and sperm that are mixed outside the woman's body in a culture dish. Any oocytes that fertilise are called embryos and these are allowed to grow for two to five days and then the best one or two are transferred into the woman's uterus. If the treatment is successful, an embryo will implant in the lining of the uterus and a fetus and placenta will develop. The woman will then be pregnant, as if she had conceived naturally.
IVF can be performed with the single oocyte that is produced naturally each month, but this is inefficient and has low success rates. Therefore, in the majority of treatment cycles, the woman undergoes stimulation of the ovaries with fertility hormones so that several oocytes are obtained.
The production of several embryos means that the best quality embryo/embryos can be replaced, thus improving success rates. It can also result in the production of ";spare"; embryos. These may be frozen to allow replacement at a later date without the need for hormone stimulation. This maximises the chance of pregnancy from one oocyte collection. This is only suitable if the embryos are of sufficient quality to survive freezing and thawing.
How commonly is IVF required?
It is important for you to realise that you are not alone. Infertility is a significant problem and the number of couples affected is often not appreciated. About one in six of all couples wanting a baby have difficulty conceiving, and in the UK around 50,000 women are treated with IVF each year. Worldwide more than 5 million"; IVF babies"; have been born.
Why has IVF been suggested to us?
IVF treatment is just one of the treatments available for fertility problems. It may be appropriate if:
- The woman has blocked fallopian tubes, endometriosis or has difficulty ovulating.
- The infertility is largely due to male factors
- The infertility is unexplained
IVF using donated oocytes may be offered to women suffering premature menopause, those whose oocytes will not fertilise, those whose ovaries have been removed or older women.
Many couples have multiple infertility problems. Each problem may be only mild and not warrant IVF on its own. However, when combined with other problems, IVF becomes the most appropriate treatment.
Why might IVF help?
IVF was originally developed to treat couples whose principle cause of infertility was tubal damage and IVF simply bypasses the tubes. However, the technique has also been found useful for a range of other conditions.
Male factor problems can be treated with IVF since a high concentration of motile sperm can be placed around each oocyte, thus helping fertilisation to occur. Very severe sperm problems can be overcome through the injection of a single sperm into the oocyte. This process is called intracytoplasmic sperm injection (ICSI).
Unexplained infertility can be treated by IVF, and may work by increasing the numbers of oocytes and embryos. This enables selection of the best embryo for replacement therefore increasing the chances that the embryo will implant.
In some cases the IVF procedure may actually uncover the cause of a couple's infertility by identifying a problem with the oocytes, sperm or embryos.
Is treatment available on the NHS?
NHS funded treatment is available for some couples, but the amount of funding and the criteria for treatment varies between different Health Authorities. These issues will be discussed with you at the time of referral.
What is the cost of treatment?
If you are not eligible for NHS treatment or do not wish to wait for treatment, you may self-fund treatment. Charges include all treatment consultations, procedures, early pregnancy monitoring and counselling. If treatment is cancelled before oocyte retrieval, there may be a refund and this information will be provided to you at your nurse appointment. Payment is required before you start your treatment cycle.
What happens before treatment starts?
1) Investigations
Fertility investigations will have been carried out in the infertility clinic prior to referral. These investigations may involve hormone tests during your menstrual cycle to ensure that you are able to produce oocytes, tests to check that your uterus is normal and a semen analysis for your partner. Further investigations may be required and these will be fully discussed with you.
a) Why are tests for HIV and Hepatitis needed?
For your own safety, the HFEA ruled in 2001 that all individuals undergoing IVF need a blood test to screen for HIV and Hepatitis B and C. This is to rule out the very small chance of any cross contamination of the viruses in the laboratory and in gamete/embryo storage vessels. Both partners must be tested. If you have a positive test, we will provide counselling and referral to a specialist for advice about your future health. These tests need to be done prior to you starting any treatment. If you are not coming through the NHS pathway, you will have to pay for these tests. Please contact the clinic for up to date prices.
Legal requirements
Confidentiality
Under the terms of the Human Fertilisation and Embryology Act (HFEA) we cannot pass on details of your treatment to anyone not covered by a treatment licence. This means that we cannot tell your GP or referring doctor about your treatment. However, we can pass on details if you provide us with written consent to disclosure. We will ask you to sign a form specifying what information may be passed on and to whom. Usually, this will be your GP, referring doctor and other people directly connected to your treatment or ongoing medical care.
During the course of treatment we have a legal obligation to collect information, including personal details, such as your name(s), date(s) of birth and some medical details. For DI treatment, but not for partner IUI, this information is passed to HFEA.
HFEA keeps a register because it has a legal obligation to tell adults, who may ask in the future, whether they were born as a result of a licensed treatment (IVF or treatment with donor sperm, oocytes or embryos).
Consent to treatment
Before beginning treatment we must also obtain your written informed consent. This means that you have been given information about the procedures, had the opportunity to receive counselling and had time to think about your decision. You may choose to change or withdraw your consent at any time before sperm is inseminated.
Welfare of the child
Before offering treatment, we are required by law to consider the welfare of any child who may be born as a result of treatment.
Preconception advice
In order to maximise the chances of conception, to help general health and improve pregnancy outcome should you conceive, you should consider the following aspects of preconception care:
- Folic acid. Supplementation has been shown to reduce the occurrence of Spina Bifida. You should take Folic acid 400 micrograms daily for three months before conception and continue this until the 12th week of pregnancy. There are special formulations of tablets for women wanting to become pregnant and these contain other vitamins, which may be useful. See your pharmacist for further advice.
- Rubella. You should make sure that your immunity to Rubella has been checked recently. Your GP will usually be able to arrange this, or it may be done through us.
- Cervical Smear. Please make sure that you are up to date with your cervical smears.
- Weight. Women who are overweight may have a reduced chance of success and you should try and make sure your weight is within normal limits before treatment. Similarly, women who are underweight have a reduced chance of success and there are additional problems posed to a pregnancy if they do conceive. BMI of between 19 and 30 is recommended.
- Smoking. If you smoke you are advised to stop before treatment not only because it may reduce the chance of treatment working, but also because of the potential effects on a pregnancy. This also applies to male partners as smoking affects sperm quality.
- Alcohol. The effect of modest alcohol consumption is not really known, but you are advised to limit yourself to less than five units a week (spread out over the week).
- Medications. If you are taking any medications, whether prescribed or not, you must tell us before treatment so we can ensure that they do not interact with any of the medications we will give you and that they will not harm a pregnancy. Please do not take any herbal or ";alternative"; remedies without checking with us first.
First appointment
At this visit the doctor will review your medical history and investigations to ensure that IVF is appropriate for you. The doctor will also explain what is involved in the treatment, what the chances of success are and the risks of treatment.
If you require further investigations, or you are not sure that IVF is the best option for you, a further appointment will be arranged before you continue with treatment. A counsellor is also available for further discussions if you wish.
Nurse consultation
The next appointment is with a fertility nurse. The purpose of this appointment is to discuss the treatment further (in particular, the timetable for treatment), be trained in how to give injections and arrange a date to commence treatment. The nurse will ensure that all necessary consent forms have been signed.
How many treatment cycles will I have?
There is no recommended set number of treatments and each time you try you increase the overall chance of being pregnant. We will offer you a review appointment after each attempt and advise you whether it is worth considering further treatment. We will also discuss with you whether there is any NHS funding available for further attempts.
What types of treatment are there?
There are a number of different drug regimes for ovarian stimulation. We will ensure that you receive the most appropriate regime for your circumstances. This will depend on a number of factors such as your age, cycle length and baseline hormone levels.
Each of the different treatment regimes is fully described in separate treatment guides. You will be given the appropriate guide for your treatment.
What happens in a treatment cycle?
The following section describes the stages in an IVF treatment cycle.
Oocyte development in the ovaries
The first step in IVF is similar to many other forms of assisted conception treatment and involves hormone stimulation of the ovaries. The hormone used is the same as that produced naturally by the body and is called Follicle Stimulating Hormone (FSH). It is administered to encourage the ovaries to produce several oocytes.
The oocytes are formed in small fluid filled sacs within the ovary called follicles. These follicles reach about 18mm in size before the oocyte is released and are easily visible on ultrasound scan. The growth of the follicles is monitored by regular ultrasound scans.
Suppression of the pituitary gland
In stimulated IVF cycles it is necessary to suppress the activity of a small gland in the brain known as the pituitary. This gland normally controls the release of two important reproductive hormones (gonadotrophins) - Follicle Stimulating Hormone (FSH) and Luteinising Hormone (LH). This process is also known as 'pituitary suppression'.
The main purpose of pituitary suppression is to prevent possible premature release (or 'surge') of LH, which would cause the early release of oocytes before they are properly mature. Without suppression this would happen in around one third of cases and lead to cancellation of the cycle. Essentially, the normal link between the pituitary and ovary is suppressed and this enables greater control over when the oocytes are released.
There are different methods of pituitary suppression. We will explain what protocol is most suitable for you and if you are to have a different drug protocol, we will discuss this with you.
Antagonist Protocol
The antagonist protocol allows your own hormones to help the gonadotrophin injections stimulate the growth of follicles in the ovaries. To stop premature ovulation a GnRH antagonist is added which directly suppresses the pituitary gland. Because the antagonist works immediately, it enables antagonist preparations to be given later in the cycle (usually from the 5th or 6th day) to suppress the possible premature LH surge.
Antagonists have the advantage of simplifying the stimulation regime and they lessen the time required to complete the cycle. Patients also experience fewer side effects and complications. Live birth rates are as good with this regime as with the long protocol. For these reasons, the majority of treatment cycles are performed with antagonists.
Long Protocol
As the name suggests, this protocol involves a longer period of injections than the antagonist protocol, and is only used in certain situations.
The treatment cycle begins with a 'gonadotrophin releasing hormone (GnRH) analogue' given daily as a nasal spray or injection. The analogue stimulates then suppresses the pituitary. The most commonly used drug is called buserelin (Suprecur).
The long protocol starts on either the second or twenty-first day of your menstrual cycle and takes around two weeks to fully suppress the pituitary. After this time you will be brought back for a scan and blood test to check suppression. Occasionally, you will require another week or two of analogue.
Once this link has been temporarily suspended, gonadotrophin preparations containing FSH (and LH if necessary) are injected each day for approximately the first ten or twelve days of the cycle. These preparations stimulate the ovaries to develop multiple follicles.
Monitoring the cycle
Your response to the gonadotrophin drugs is monitored carefully with regular vaginal ultrasound scans. In addition, depending on the treatment protocol, some blood tests may be required to measure specific hormone levels.
If too few follicles are developing or there is an unexpected change within the lining of the uterus, the chances of pregnancy in that particular cycle may be reduced. It may be necessary to stop treatment and possibly adjust the treatment protocol in subsequent cycles.
Triggering final oocyte maturation
The time of final oocyte maturation can be decided by triggering this using a hormone injection. When follicles have reached the requested size (usually after 10 to 14 days), a different hormone injection is given which releases the oocytes from the side wall of the follicle.
The hormone injection is carefully timed 36 hours before oocyte retrieval. As this is done in the morning, this last injection is given late at night two days before.
Occasionally the ovaries become too stimulated and this increases the risk of Ovarian Hyperstimulation Syndrome (OHSS). We would normally recommend a change in the treatment regime to involve the use of a different drug to trigger final oocyte maturation. We will still proceed with retrieving your oocytes although we may advise you to 'freeze all' your embryos for some to be replaced in a frozen embryo transfer cycle. This is to maximize the chances of pregnancy and minimize the risks of developing severe OHSS.
You should report any abnormal pain or sickness as these may be signs that excessive stimulation is occurring. Please see the section at the end of this leaflet for further information about this condition.
Oocyte retrieval
The day of egg collection is known as day 0 when referring to embryo development. Just before the follicles ovulate, the fluid within the follicles is collected by ultrasound guided oocyte retrieval. This is carried out on a day-care basis and is usually done under conscious sedation (with an anaesthetist) at our clinic. A fine hollow needle is passed, under ultrasound guidance, through the vagina to the ovaries and each large follicle is drained. The procedure takes about 15 to 30 minutes.
You will rest in the clinic for a short while following the procedure after which you may go home. You will be a little drowsy from the sedative drugs. You must be taken home and must not drive or operate machinery for 24 hours.
Very occasionally, despite a satisfactory scan, no oocytes are collected. In such circumstances the reasons for this would be discussed with you as soon as possible.
Sperm collection
At the same time as the egg collection the sperm will be prepared. If you are using partner sperm, your partner will be asked to produce a sample at the clinic. This may be before, after or during your egg collection. If you are having treatment with donor eggs your partner will be given an appointment time. If frozen partner sperm or donor sperm is used, this will be thawed.
Only the best quality, swimming sperm will be used in your treatment. Occasionally if there is a problem with the sample on the day of egg collection, the embryologist may recommend ICSI instead of IVF. This will be discussed with you at the time.
Normal intercourse throughout your cycle will not interfere with your treatment. However, a period of abstinence of 2 to 5 days is recommended before producing the sample to ensure the best possible sperm quality.
If you anticipate any problems with producing a sample at the clinic, please contact the embryology team well in advance of your treatment, so that a back up sperm freeze can be arranged.
Insemination and fertilisation
After collection, the oocytes are placed in an incubator. IVF takes place in the afternoon on the day of egg collection. All of your eggs will be left overnight with tens of thousands of swimming sperm in a drop of fluid containing all of the nutrients they need. If ICSI is required, a single sperm will be injected directly into each mature oocyte. Later in this leaflet, ICSI will be discussed in more detail.
The signs of fertilisation appear 16-18 hours after the sperm and egg come into contact with each other (post-insemination, pi). The embryologists check for fertilisation first thing the morning after egg collection (day 1 of embryo development). Normal fertilisation is denoted by the presence of two pronuclei: one containing genetic material from the sperm and one from the egg.

A normally fertilised embryo displaying two pronuclei 18 hours after insemination
We usually expect around 60-70% of mature eggs to fertilise. When surgically retrieved sperm is used the fertilisation rate can be lower. After the fertilisation check has been performed, the embryologist will telephone you to let you know the results and make a plan for the rest of your treatment.
Occasionally an embryo may display just one pronuclei or three or more pronuclei. These embryos are developing abnormally and are not suitable for use in treatment, but can be donated to research or training. Very occasionally none of the eggs fertilise. If this is the case in your treatment the embryologist will discuss this in full with you.
Embryo development
Your embryos will be kept in the lab for up to six days. The major developmental milestones are as follows:
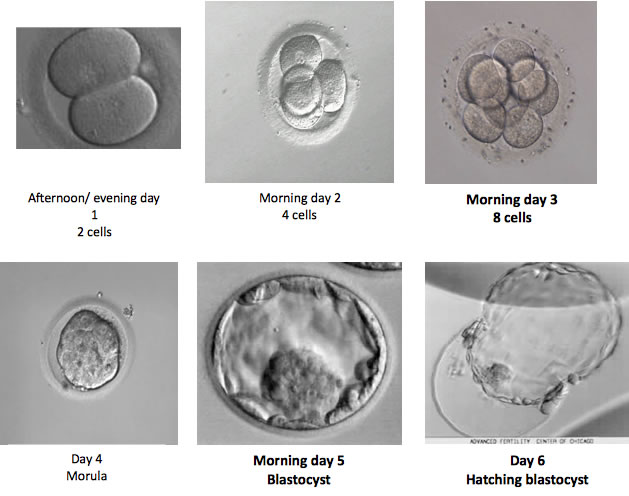
The embryos are usually checked on day 3, day 5 and day 6 of development and we will speak to you by phone or in person at the clinic on these days to update you on the embryos' development. We do not routinely check embryos on day 2 or day 4 of development and do not contact you on these days.
The embryologists can tell an embryo's potential to establish a pregnancy by monitoring its development and looking at the number, shape and size of its cells over the course of a few days. This information is used to give them a grade, which enables the embryos to be ranked in order of quality. It is then possible to select the best one or two embryos for transfer, and any other good quality embryos for freezing.
Timing of embryo transfer
Your embryo transfer may take place on day 2, 3 or 5 of development. The day of transfer will depend on several factors, including:
- How many embryos have fertilised
- Your age / the age of the egg donor
- The development of your embryos in the current treatment cycle
- Embryo development in any previous treatment cycles
Each case is treated individually and your personalised treatment plan will be discussed with you by an embryologist during your fertilisation results phone call. Occasionally the plan may change as we observe your embryos' development, but we let you know as soon as possible if this is the case.
Blastocyst culture
If you have three or more embryos that have fertilised, we may recommend that you keep all the embryos in the lab for five days before performing the embryo transfer. This is known as blastocyst culture.
A blastocyst is the most advanced stage of embryo development that we observe in the IVF laboratory. In order to reach this stage the embryo must grow from 8 cells to 100s of cells in the space of just 48 hours. We know that an embryo must reach this advanced stage of development in order to establish a pregnancy. However, we also know that not every fertilised embryo is capable of developing to this stage.
Keeping the embryos in the lab for five days before transfer or freezing allows the embryologists to see which embryos are capable of reaching this advanced stage of development, and therefore which embryos are going to give you the best chance of pregnancy.
Blastocyst culture does not change the embryos in any way, nor does it improve or decrease their potential for establishing a pregnancy. We do not expect every embryo from the group to develop to the blastocyst stage; this is normal. Very rarely we see patients that do not have any embryos that make it to the blastocyst or morula stage, and therefore have no embryos suitable for transfer. If this is the case, the evidence suggests that none of these embryos would have been capable of making a pregnancy. The embryologist will discuss all of this with you.
Sometimes after the fertilisation check we may recommend blastocyst culture and plan for your transfer to be on day 5, but then when we check the embryos' development on day 3 we find that actually one or two of the embryos are already clearly developing better than the others. In this case, your transfer may be brought forward to day 3. This will not affect your chances of pregnancy.
Blastocyst culture is only usually recommended for patients that have a group of embryos to choose from. For patients that have one or two fertilised embryos we normally recommend day 2 or day 3 transfer.
Freeze all
We normally recommend blastocyst culture for patients having a ";freeze all"; cycle. This way, we freeze only the embryos that are proven to be of good quality for use in your future treatment. We do not expect all the embryos to reach the blastocyst stage and be suitable for freezing; this is normal. There is a risk that there will be no embryos suitable for freezing, but this is very rare. The embryologist will discuss all of this with you during your fertilisation results phone call.
Embryo transfer
The embryo transfer procedure is usually straightforward and completely painless. An abdominal ultrasound scan is used to visualise your womb. The embryos are then placed into the womb by passing a fine plastic tube (catheter) through your cervix. The procedure will take around 15 minutes and does not require any sedation or other medication.
Spare embryos
There may be surplus embryos following treatment and you should think about what you would like to happen to these. Briefly, they may be frozen for future treatment, donated for research or allowed to perish. Further information about your choices is found at the end of this leaflet. The embryologists will advise whether any remaining embryos are suitable for freezing for treatment. You will find further information about embryo storage at the end of this leaflet. Freezing of ";spare"; embryos will result in an additional charge if your treatment is not NHS funded.
Witnessing
As an HFEA-licensed fertility centre, we comply with very strict regulations regarding labelling and witnessing of sperm, eggs and embryos. Everything is labelled with three unique identifiers: your name, date or birth and hospital number. These details are checked by an embryologist and our advanced electronic witnessing system at all stages of your treatment. At critical stages, including insemination, we also have a second embryologist double checking the details. A record of all the witnessing checks is kept in your notes.
Hormone support
In the second half of the cycle the lining of the uterus (endometrium) has to be supported with progesterone to help the embryo implant in the uterus. This is called ";luteal phase support"; and ensures that the endometrium undergoes the necessary changes to allow implantation of an embryo. The method of support will depend upon the levels of hormones already in the blood and the type of drugs that have already been given. In order to check that the hormone levels are correct we may ask you to have a blood test around the time of embryo transfer.
What happens if the pregnancy test is positive?
Pregnancy scans
You will be asked to attend for a vaginal scan about five weeks after your IVF/ICSI (this is equivalent to seven week pregnancy).
This scan is important to ensure that the pregnancy is in the correct place, that it is developing normally and to confirm how many pregnancy sacs there are. At this stage, the pregnancy should be clearly visible inside the uterus as a small sac with a tiny fetus within. It should be possible to identify a heartbeat at this stage.
If all is progressing normally, you will be asked to attend antenatal care. If problems are identified during these scans we will discuss the findings with you and make appropriate plans.
You should continue taking folic acid until 12 weeks of pregnancy.
Pregnancy outcome
We are required by law to notify HFEA of the outcome of all treatment cycles. Please report the outcome of the pregnancy back to us. More information regarding this will be given to you when a pregnancy is confirmed.
What happens if the pregnancy test is negative?
A negative result means that pregnancy has not occurred this time. We realise that you may be very disappointed and the staff at the clinic are always available to offer support and advice. The counsellor is also available should you wish to have an appointment.
Issues to Consider with IVF
There are a number of issues that you may need to consider before starting treatment.
Parental responsibility
Any child born as a result of treatment will be legally the child of the husband or male partner, his name should be put on the birth certificate as the legal father. We will obtain written consent from the male partner acknowledging that you are being treated together.
Where a child is born to an unmarried couple, the male partner may not have parental responsibility for that child under the Children Act 1989. Unmarried couples are advised to seek their own legal advice about the male partner's rights and responsibilities towards any child who may be born as a result of treatment. Should both partners wish each other to be recorded as legal parents it is important that the necessary forms are completed before treatment starts. If in doubt please ask us.
What is the chance of success?
Your own chance of success will be influenced by a number of factors and may be different to the overall results. We will discuss these issues with you before you start treatment. For up to date national statistics please refer to www.hfea.gov.uk and for recent data from our clinic please refer to our success rates.
There are many factors that influence a woman's chances of having a live birth. Important factors include the following:
- The age of the woman. The main influence on the success of treatment is the age of the woman. The chance of success decreases with age.
- Previous pregnancies. Women who have been pregnant before, or who have had a previous IVF birth, have a higher chance of conceiving with IVF treatment.
- The duration of infertility. The live birth rate is lower the longer a couple has been infertile. This effect is most marked in long-standing infertility, whatever the age of the woman.
- Previous IVF attempts. The live birth rate is highest at the first IVF attempt. For this reason we advise that each cycle is reviewed before embarking upon further treatment.
- Number of embryos replaced. We will always advise you to have one embryo replaced if you have good quality embryos.
Elective single embryo transfer (eSET) involves selecting one embryo for transfer from a larger number of available embryos. eSET helps women avoid several risks to their own health that are associated with carrying a multiple pregnancy. It also helps families achieve success while preventing some risks known to be associated with giving birth to twins or what is called ";high order multiple births"; (three or more children born at the same time). Infants born in multiple births are more often born early (preterm), are smaller (low birth weight) and experience more adverse health outcomes than singleton infants. There is consensus among experts that the desired outcome of ART is a healthy singleton infant.
Research has found that among women with a good chance of success with ART, those who chose to have a single embryo transferred had a similar number of live-birth deliveries compared to those who chose to transfer multiple embryos, but almost all of the infants they delivered were singletons.
In our clinic, single embryo transfer is considered appropriate for patients with good prognosis, usually women aged 37 years or younger and with embryos of good quality.
Is there an increased risk of a multiple pregnancy?
While the prospect of twins or triplets may seem attractive, there are many serious risks associated with a multiple pregnancy. Research has shown that multiple pregnancies can lead to a higher risk of:
- Complications during pregnancy
- Premature birth and low birth weight
- Disability
- Death of infants or within 28 days of birth (known as neonatal death)
In addition to the serious risk to the babies' health, a multiple birth can create enormous strain for the parents, including financial difficulties as well as emotional and physical exhaustion. In some cases, the joys of parenthood are greatly reduced by these problems.
Are there any other risks of an IVF pregnancy?
There is an increased risk of a pregnancy in the fallopian tube (ectopic). This is why the early pregnancy scans are important to establish where the pregnancy is and that a heartbeat is present.
In addition, there is a very small chance of having one pregnancy correctly placed in the uterus and another in the tube. This is called a heterotropic pregnancy. It is very rare with naturally conceived pregnancies (around 1 in 10,000), but can occur slightly more frequently with IVF. However, it is still very uncommon. Nevertheless, you should always contact us if you are pregnant and have pain or bleeding in the early stages, even if scans have shown a pregnancy in the uterus.
There is always a small risk (around 2%) that a baby will have some abnormality and IVF does not protect you from this, but the chances are certainly no greater than for a natural conception.
Does oocyte retrieval have any risks?
Oocyte retrieval is a surgical procedure and, as such, has a few risks from anaesthesia (or sedation), bleeding and introduction of infection. However these risks are extremely small and significant problems occur in less than 1:2000 patients.
Ovarian Hyperstimulation Syndrome (OHSS)
The drugs used to stimulate the ovaries can occasionally cause the ovaries to over respond and this can lead to a potentially serious condition called ovarian hyperstimulation syndrome (OHSS).
How often does OHSS occur?
Significant OHSS affects less than 1% of women undergoing treatment, but it can be serious if appropriate treatment is not given. In it's most severe form, or if left untreated, it can be life threatening.
Once you start your treatment cycle it is important that you know the symptoms of this condition and how to contact members of the medical team if you need them.
What is OHSS?
The ovaries become large and cystic with leakage of fluid into the abdomen. This causes swelling and discomfort. The leakage of fluid can cause dehydration and this can make the blood more likely to clot and can affect the way the kidneys and other organs work.
Fortunately most cases of OHSS are usually mild to moderate, but in a few cases, if left untreated, it may become severe. If a patient who suffers OHSS becomes pregnant, the pregnancy hormones produced by the baby may make the condition temporarily worse.
Why does OHSS occur?
The condition occurs because the ovaries produce too many follicles and have high levels of oestrogen. Therefore, women whose ovaries respond more to the drugs are at an increased risk of developing OHSS.
Who is at risk of OHSS?
Any woman undergoing stimulation of the ovaries is at risk, but some are at greater risk than others. Younger women and those with polycystic ovaries are more at risk and we tend to use lower doses of drugs in these women to minimise the risk.
Careful monitoring during the treatment cycle can often predict the risk of OHSS in some women. If an increased risk is identified, treatment cycles may be either cancelled or modified to prevent the condition occurring. Some of these changes may have cost implications for self-paying patients that cannot be foreseen or predicted. These will be discussed in your medical/nursing consultations in the clinic.
Despite all these precautions, it is not always possible to prevent the condition and it may occur in some women who do not appear to have over responded.
When does OHSS occur?
The condition only occurs after the injection of hCG (late night injection). If you have symptoms before embryo transfer, the embryos can be frozen and the transfer delayed to allow the condition to subside on its own.
What are the symptoms of OHSS?
| Mild OHSS | Moderate OHSS | Severe OHSS |
| • Abdominal swelling • Lower abdominal pain • Nausea (feeling sick) |
• Mild symptoms plus: • Diarrhoea • Vomiting • Dark strong urine |
• Moderate symptoms plus: • Persistent vomiting - unable to tolerate any fluid orally • Gross abdominal swelling resulting in shortness of breath |
You will not necessarily develop all the symptoms at the same time
What should I do if I think I have OHSS?
You are advised to contact us if you develop any of the above symptoms or feel unwell. If left untreated OHSS can become severe.
It is important to drink plenty of fluids to avoid becoming dehydrated. Dark strong urine is an indication of dehydration. You can take paracetamol (maximum 8 tablets in 24 hours) for pain relief.
Mild OHSS may be relieved by these simple measures, but you should contact us for advice. Sometimes hospital admission is necessary to ensure adequate fluid intake (either orally or through a drip) and adequate pain relief.
Who should I contact?
Since OHSS is uncommon, your GP or local hospital may not be used to dealing with this condition. Therefore you are advised to contact us directly.
During working hours (Monday-Friday 8am to 4pm) contact 02381 20 6980. Out of working hours, leave a message and we will return your call the following working day.
If you are in treatment and need urgent medical advice out of hours, call our on-call nurse on 07767463126. Please only use this if your need is urgent.
Information for patients requiring ICSI
You may have been advised that your IVF treatment needs to be combined with sperm microinjection. This section outlines the principles of ICSI, but if you have any further questions please do not hesitate to contact one of our embryologists.
What is ICSI?
ICSI is a type of IVF treatment that involves the injection of a single sperm into each mature oocyte. Normally fertilised embryos are then cultured in the laboratory as in a conventional IVF cycle.
ICSI was introduced into clinical treatment for certain types of infertility in 1992 and has results that are very similar to conventional IVF.
What does ICSI involve?
ICSI is similar to conventional IVF in that oocytes and sperm are collected from each partner. To achieve fertilisation, a single sperm is taken up in a fine glass needle and is injected directly into an oocyte.
The oocytes are incubated and examined the following day for fertilisation. As in conventional IVF, embryos are cultured in the laboratory and an embryo may then be transferred back into the uterus of the woman.
Not all oocytes collected will be of a high enough quality or mature enough to be suitable for injection. In addition, some oocytes may not survive the injection process. In our clinic, this is less than 5% of all injected oocytes.
When is ICSI used?
In conventional IVF the oocytes and the sperm are mixed together in a dish and the sperm fertilise the oocytes naturally. ICSI is used when sperm are unable to fertilise the oocyte naturally. It bypasses the natural processes involved in a sperm penetrating an oocyte. ICSI may be used in the following cases:
- When the sperm count is very low
- When the sperm cannot move properly
- When the sperm have high rates of abnormal forms
- When sperm has been surgically retrieved from the epididymis (PESA) or the testicles (TESA), from the urine, or by electroejaculation
- When there are high levels of antibodies in the semen
- When fertilisation has failed in previous IVF treatment
Are there any risks with ICSI treatment?
ICSI may use sperm that would not otherwise be able to fertilise an oocyte. This has raised concerns about the potential risks to children born as a result of ICSI. Several follow-up studies have now been published, but ICSI is still a relatively new technique, and all children conceived using ICSI are still very young. Consequently, these follow-up studies involve relatively small numbers of children and do not include effects that may only be seen in older children or in the next generation. More studies are needed to confirm the longer term safety of this procedure.
The use of ICSI has been potentially linked with certain genetic and developmental defects as explained below:
1) Possible inheritance of genetic and chromosomal abnormalities.
- Inheritance of cystic fibrosis gene mutations. Some men who have no sperm in their semen are found to have congenital bilateral absence of the vas deferens (CBAVD). In this condition, the tubes that carry sperm from the testes to the penis are missing. Two thirds of men with CBAVD are also carriers of certain cystic fibrosis mutations. If you are a carrier of this condition it will not cause you any other health problems. About 1 in 25 of the wider population may also carry the mutation. This means that if your partner also happens to be a carrier of the mutation, there is a chance that a child born through treatment may have cystic fibrosis. For this reason we offer men with low sperm counts and their partners genetic counselling and testing before proceeding with ICSI treatment.
- Sex chromosome defects and the inheritance of sub-fertility. Chromosomes are the structures in the cell that carry the genetic information. We have 46 chromosomes in each cell (2 pairs of 23 chromosomes). Men have one X and one Y chromosome in each cell. Some genes on the Y chromosome are involved in sperm production. A small number of sub-fertile men have parts of the Y chromosome missing and this may be responsible for their fertility problem. This means that using sperm with such deletions to create an embryo may result in the same type of fertility problem being passed from father to son.
Some men with subfertility have also been shown to have a higher chance of having an abnormal number of chromosomes, in particular the sex chromosomes (X and Y). It is estimated that up to 2.4% of the wider population have a chromosomal abnormality, but up to 3.3% of fathers of ICSI babies have abnormal chromosomes.
Babies born from ICSI treatment may have a slightly increased risk of inheriting these abnormalities. Because of this, we examine the numbers of chromosomes in all men requiring ICSI.
2) New chromosomal abnormalities.
Oocyte and sperm production is a very complex process and this means that even if an individual possesses a normal number of chromosomes, their oocyte or sperm could potentially have an abnormal number. It is not possible to detect which oocytes or sperm have chromosomal abnormalities, and oocytes or sperm that might not have been able to fertilise naturally could therefore be used in ICSI. Babies born after ICSI have been reported to have new chromosomal abnormalities in up to 3% of cases. The rate in the general population is around 0.6%.
3) Possible developmental and birth defects.
- Birth defects. There is no clear evidence whether ICSI results in higher rates of birth defects. The number of babies reported to have major birth defects, such as cleft palate, is between 1% and 5% in both the general population and in babies born following ICSI. Studies suggest that minor abnormalities occur in up to 20% of ICSI babies, compared to up to 15% of the population. More studies are needed to establish whether there is an increased risk.
- Developmental delays. One recent study that followed up a relatively small number of children has given an indication of possible delays in mental development at one year of age in some children born following ICSI. Other studies have not shown this link and further research is needed in this area.
4) Possible risks during pregnancy.
With ICSI it is possible that abnormal sperm that would not usually be able to produce a viable embryo, could be used, increasing the chance of an abnormal embryo being formed. Many abnormal embryos will not implant into the uterus and grow, but some might. This may lead to a possible higher risk of miscarriage. It has been reported that the risk of miscarriage increases in proportion to the severity of male infertility.
Embryo Freezing and Storage
What is embryo freezing and storage?
In a cycle of IVF treatment, more embryos are often created than can be replaced in the woman's uterus in one treatment cycle. You should consider what you wish to happen to any spare embryos that may be created
It is important to select the best embryos for your transfer, but if good quality embryos are left over, these can be frozen for subsequent use. This may avoid the need for repeated drug stimulation, oocyte retrieval, sperm collection and insemination. The embryologist will only recommend that good quality embryos at the correct stage of development be frozen (usually at the blastocyst stage on day 5 or day 6). This is to give you the best chance of success. Around 50% of patients have spare embryos that are suitable for freezing after they have had their embryo transfer. In rare circumstances it may be suggested that you freeze all your embryos before transfer if you are at risk of ovarian hyperstimulation syndrome.
It is possible to store embryos for use in future treatment by freezing them at very low temperatures in tanks of liquid nitrogen. The embryos are stored in sealed, labelled straws in locked storage containers. The freezing and thawing of embryos has to be carried out very carefully. In order to protect the embryos in the freezing process a liquid called a cryoprotectant is used. Despite the precautions that are taken, not all embryos survive the freezing and thawing process and the live birth rate per cycle from frozen embryos is usually lower than fresh embryo transfers.
Although freezing of embryos is carried out very carefully, due to the nature of the process and the methods used to store the embryos, there is a remote possibility of loss of stored embryos during the process of freezing, storing and thawing.
Should any remaining embryos not be required for further treatment, they can be donated for the treatment of others, to research or allowed to perish. You and your partner must both provide consent as to the use of these embryos. Your consents must agree before an embryo can be used or donated for treatment or research.
How long can embryos be stored?
Embryos are stored according to you and your partners consent. This period may be extended in blocks to a maximum storage period of 55 years on confirmation that the individual's fertility is still impaired by any previous treatment/surgery.
We carry out regular reviews of the embryos that we have in storage and will remain in contact with you annually by letter. It is of vital importance that you keep us informed of any changes of address and respond promptly to any correspondence that we send you. This will enable us to ensure that you have plenty of time to deal with any issues arising from the storage of your embryos.
If at the end of you initial consent period we are unable to contact you, we will have to allow your embryos to perish.
How are stored embryos used in treatment?
Embryos may be transferred in either a natural or hormone replacement cycle. In a natural cycle the woman's cycle is monitored carefully to time when she produces an oocyte. The date at which the lining of the uterus (endometrium) will allow implantation of the embryo can then be calculated. The embryo(s) can than be thawed and embryo transfer performed as in a fresh IVF cycle. Alternatively, hormones may be used to build up the endometrium to allow implantation. Natural cycles are simpler, but are only suitable if the underlying function of the ovaries is good.
What consent is required?
You can only store your embryos if both you and your partner have completed the HFEA consent forms. A nurse will explain these forms at your consultation appointment.
Are there any risks to freezing embryos?
The embryologist will only select good quality embryos to freeze as these embryos have the best chance of survival. Studies have demonstrated that children born as a result of treatment using frozen embryos appear to be as healthy as those children born as a result of fresh embryo transfer cycles.
What costs are involved?
The cost for embryo freezing and subsequent treatment cycles can be found in the treatment charges leaflet. The cost for initial freezing also includes the first year's storage. There is an annual charge for continued storage of your embryos to cover the costs of maintaining the storage tanks and the administrative costs involved.
Using Human Embryos for Research
We firmly believe that it is through world class research that one can significantly improve reproductive health. We receive external funding from charities and government organisations to conduct important research in different aspects of reproduction.
Embryos that are surplus to the needs of your fertility treatment can be donated for research. If you do agree to donate your embryos, we only use embryos that you no longer require for your own treatment or that are unsuitable for your treatment.
Why donate embryos for research?
Any area of clinical treatment needs a firm backing in scientific research and human assisted reproduction is no exception. We do not yet understand all the factors involved in the development of the embryo in the laboratory and factors involved in implantation after embryo transfer. Scientific research led to the IVF treatment you will receive and research in the future will lead to improved methods of treatment. This type of research cannot be done using animal embryos because they are substantially different from human embryos.
Who regulates embryo research?
The Human Fertilisation and Embryology Authority (HFEA) encourages research while ensuring that it is carried out responsibly and for good reason. Therefore, the HFEA must license all research projects that involve the creation, storage or use of human embryos outside the body.
What kind of research is allowed?
For a research licence to be granted the HFEA must be satisfied that the use of human embryos is 'necessary or desirable' for at least one of the following purposes:
- To promote advances in the treatment of infertility
- To increase knowledge about the causes of congenital disease
- To increase knowledge about the causes of miscarriages
- To develop more effective techniques of contraception
- To develop methods for detecting the presence of gene or chromosome abnormalities in embryos before implantation
What kind of research is not allowed?
While encouraging research, the Human Fertilisation and Embryology Act specifically prohibits certain activities involving human embryos. These include:
- Keeping or using an embryo after the appearance of the primitive streak (thickening in surface of embryos which results in the first clearly recognisable stage in embryonic development) or after 14 days, whichever is earliest.
- Placing a human embryo in an animal
- Altering the genetic structure of any cell while it forms part of an embryo
- Using embryos for any other purposes except in pursuance of a licence
How are embryos obtained for research?
During IVF treatment oocytes will be inseminated with sperm to try to create embryos. Any embryos unsuitable for transfer or freezing are normally allowed to perish. You may be asked to allow the use of these embryos, which would normally be discarded, in research.
If you have frozen embryos that you no longer require for your treatment, you may also donate these for research.
Is information provided about the research that the can be done?
We will inform you about the specific type of research project that will be undertaken on your embryos and you will receive a separate information leaflet giving more details about the study. You have the opportunity to ask questions and discuss the study. You will be asked to give specific consent to the research study.
What type of research is being done in Southampton?
We want to know more about how best to grow embryos in the laboratory and to understand how they implant in the uterus. Embryos will be grown for a few days in culture in the laboratory with some cells from the uterus. In this way we can investigate the biochemical signals between the embryo and uterine cells that regulate implantation. Cells from the embryo may also be cultured to grow 'stem cells', some of these form cells of the placenta (trophoblast cells), which will be used to investigate the causes of implantation failure. All the research is fully approved and licensed by HFEA.
What will happen to the embryos after the research?
Human embryos can only be used for research for the first 14 days of their development. At this very early stage the embryo is simply a small ball of cells about the size of a pinhead. At 14 days we are obliged to destroy all embryos.
Any embryos used or created for the purposes of research will not be transferred in a treatment cycle.
Do embryos have to be donated to research?
You are under no obligation to donate your embryos to a research project. You have the right to vary or withdraw your consent from the study at any time up until the time the embryos are used.
Your decision whether or not to donate embryos to research will not compromise your treatment in any way.
What consent is required?
You will be asked to sign two separate consent forms. The statutory consent form (provided by the HFEA) requires us to obtain your general consent for use of your embryos in research. This form allows you to specify conditions subject to which your embryos may be used. You will also be asked to complete a consent form following full discussion about the study involved. Both partners will be required to give consent.
Will any further research be carried out on the embryos?
The majority of research undertaken is carried out on embryos that will be discarded when the particular study is complete. However, it is possible that embryos or embryo cell samples may be preserved or fixed (which renders the embryos non-viable) for future studies.
Research on these embryos is called secondary research. The HFEA has no remit over the regulation of research on non-viable embryos. However, we would inform you of any secondary research that might be carried out on your embryos and the implications of this.
Where can we get further information?
We hope that this information leaflet has given you all the information that you require before your treatment. Please do not hesitate to contact us if you need further information or if you do not understand anything. We welcome any suggestions you may have on improving our leaflets.
The staff of the clinic are always available should you require any further information and this includes 24 hour out-of-hours cover should you have a more serious problem.
A list of national and local Infertility Support groups is available in the clinic.
Further information can be also obtained from the Human Fertilisation & Embryology Authority (HFEA). Please visit www.hfea.gov.uk for information on infertility, treatment and advise on how to choose your fertility clinic.
TESTIMONIALS
Mr Brook, helpful, kind manner, explain things in an easy to understand way. Gave me confidence in my treatment.


